Aging is associated with functional declines throughout the body, including some aspects of cognitive performance. However, there are marked individual differences in age-related cognitive changes, and the factors that contribute to this variability are the subject of vigorous debate. Recent evidence suggests that the hormonal and metabolic environment may modulate these age-related cognitive changes. Several hormonal systems have been implicated as modulators of individual differences in cognitive decline and development of dementia and in my work I have focused on gonadal (e.g. testosterone) and adrenal (e.g. cortisol) steroids . A more recent interest is in how insulin regulatory mechanisms may impact cognitive and brain aging.
Stress and Cortisol and Cognitive Aging
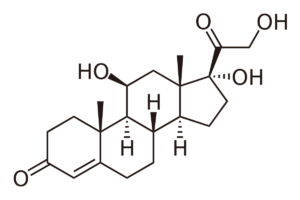
One candidate hormone involved in cognitive and brain aging in humans is the adrenal steroid cortisol. Cortisol is a major glucocorticoid which thus regulates blood glucose levels and is the major steroid mediating the stress response. There is considerable evidence from animal research that chronic exposure to high levels of corticosteroids causes atrophy of the hippocampus and contributes to age-related declines in memory. In humans, evidence is now accumulating suggesting that similar adverse effects may accompany excess cortisol exposure, particularly in vulnerable populations such as the elderly. For example, cortisol levels have been found to be higher in individuals with dementia and high cortisol levels have been found to be associated with hippocampal atrophy and memory loss. My contributions in this area include the demonstration that high levels of cortisol are associated with an increased risk for Alzheimer’s disease and that the cortisol awakening response is related to memory and cognitive function.
Ennis GE, An Y, Resnick SM, Ferrucci L, O’Brien RJ, Moffat SD. (2017). Long-term cortisol measures predict Alzheimer disease risk. Neurology. 2017 Jan 24;88(4):371-378. PDF
Ennis GE, Quintin EM, Saelzler U, Kennedy KM, Hertzog C, Moffat SD. Cortisol relates to regional limbic system structure in older but not younger adults. Psychoneuroendocrinology. 2019 Mar;101:111-120. PDF
Testosterone and Cognitive Aging
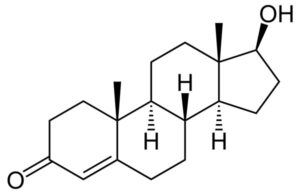
In men, testosterone (T) levels decline precipitously between the ages of 30 and 80; results from both epidemiological research and T replacement studies suggest that the progressive decline in T secretion in aging men contributes to selective losses in memory and cognitive function. My major contributions to this field are large longitudinal studies which have shown that men who maintain high endogenous testosterone levels as they age have lower risk for Alzheimer’s disease, lower risk for cognitive decline and increased hippocampal blood flow as assessed by O15 PET studies.
Moffat, S.D., Zonderman, A.B., Metter, E.J., Kawas, C., Blackman, M.R., Harman, S.M & Resnick, S.M. (2004). Free testosterone and risk for Alzheimer’s disease in older men. Neurology 62: 188-193. PDF
Moffat, S.D. & Resnick, S.M. (2007). Long-term free testosterone levels predict regional cerebral blood flow patterns in elderly men. Neurobiology of Aging 28: 914-920. PDF
Insulin and Glucose Regulation
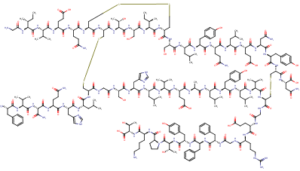
Diabetes or insulin dysregulation is highly prevalent in the US population with more than 50% of older adults being affected. This is concerning for multiple reasons, including the observation that diabetes is a risk factor for Alzheimer’s disease and cognitive decline. This area of research in the Moffat lab examines insulin and glucose metabolism using advanced and sensitive measures of pancreatic beta-cell function and insulin sensitivity. We examine the impact of glucose and insulin regulation to age-sensitive cognitive domains and MRI measures that assess not only neural structure (MRI) but also neural function (fMRI) and neural physiology (ASL cerebral blood flow).
Ennis, G.E. Saelzler, U.G., Umpierrez, G. & Moffat, S.D. Prediabetes and working memory in older adults. Brain and Neuroscience Advances. In press.